Abstract
Introduction: Essential thrombocythemia (ET) is a chronic myeloproliferative neoplasm characterized by clonal platelet production and an increased risk for thrombotic and hemorrhagic events. Limited real-world data exist regarding the clinical characteristics and treatment patterns of ET in the United States; most prior data have been generated outside the United States. The Myelofibrosis and Essential Thrombocythemia Observational STudy (MOST) is an ongoing observational study being conducted to describe contemporary demographics, burden of disease, clinical management, and patient-reported outcomes in patients with specific risk categories of myelofibrosis (MF) or ET in the United States. This analysis describes the clinical characteristics of patients with ET currently enrolled in MOST.
Methods: MOST is a multicenter, noninterventional, prospective, observational study in patients with a clinical diagnosis of specific risk categories of MF or ET (NCT02953704). Eligible patients with ET included high-risk patients (≥ 60 years of age and/or a history of thromboembolic events [TEs]), or low-risk patients currently receiving ET-directed therapy. Key exclusion criteria included participation in blinded investigational drug studies, life expectancy ≤ 6 months, or diagnosis of other malignancy. Data regarding disease and clinical characteristics are collected at usual-care visits over a planned 36-month observation period. Patient demographics and clinical characteristics at enrollment were described with descriptive statistics.
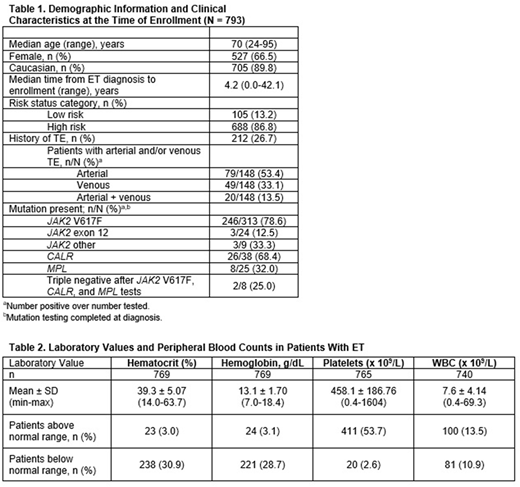
Results: At data cutoff (May 18, 2018), 793 eligible patients were enrolled from 85 sites since November 29, 2016. The median age at enrollment was 70 (range, 24-95) years, 66.5% were female, and 89.8% were Caucasian. The median time from ET diagnosis to enrollment was 4.2 (range, 0.0-42.1) years with a proportion of patients diagnosed within 1 year (19.5%), 1 to < 5 years (35.0%), 5 to < 10 years (21.7%), or ≥ 10 years (23.8%) of enrollment. Approximately 40% of patients were retired and 42.7% were working full- or part-time at enrollment. A total of 212 patients (26.7%) had a history of TE at the time of enrollment. The type of TE was available for 148 patients, the most common was arterial events (53.4%); 33.1% had venous, and 13.5% of patients had both arterial and venous events. Six hundred and eighty-eight patients (86.8%) were classified as high-risk. Assessments at the time of ET diagnosis, among evaluable patients, included bone marrow biopsy (51.4%; 393/765) and mutational testing (77.2%; 590/764). Three hundred and forty-nine patients had mutation test results reported at the time of diagnosis; of patients with JAK2 V617F test results reported at the time of diagnosis (n = 313), 78.6% were positive for JAK2 V617F (Table 1). Laboratory values and peripheral blood counts were reported for patients with available data (Table 2). The majority of patients (87.9%) had received at least 1 ET-directed therapy prior to enrollment, which in some cases was the same medication the patient was receiving at the time of enrollment. At the time of enrollment, 740 patients (93.3%) were receiving at least 1 current ET-directed therapy, including HU (71.6%; 530/740), anagrelide (13.1%; 97/740), ruxolitinib (4.7%; 35/740), interferon (3.0%; 22/740), and busulfan (0.3%; 2/740). Of 793 patients, the most frequently occurring relevant comorbid conditions were hypertension (52.7%), history of smoking (44.7%), and hyperlipidemia (24.1%). Among 761 patients with ET-related symptoms assessed at diagnosis, the most common symptoms documented by healthcare providers included constitutional (22.9%), vasomotor (16.0%), and spleen-associated symptoms (3.9%), and pruritus (2.6%).
Conclusions: Prior real-world data in ET has predominately been generated outside of the United States or has been reported from single institutional experiences. The MOST study will provide a more complete picture of the patient characteristics and outcomes of patients receiving ET-directed therapy in the United States. Ultimately, these data will be important for determining ET treatment gaps and areas of unmet need.
Yacoub:Cara Therapeutics: Equity Ownership; Inycte: Honoraria, Speakers Bureau; Novartis: Honoraria, Speakers Bureau; Ardelyx, INC.: Equity Ownership; Seattle Genetics: Honoraria, Speakers Bureau; Dynavax: Equity Ownership. Verstovsek:Novartis: Membership on an entity's Board of Directors or advisory committees, Research Funding, Speakers Bureau; Italfarmaco: Membership on an entity's Board of Directors or advisory committees; Celgene: Membership on an entity's Board of Directors or advisory committees; Incyte: Consultancy. Shao:ASH: Membership on an entity's Board of Directors or advisory committees; ASCO: Membership on an entity's Board of Directors or advisory committees. Agrawal:Incyte: Speakers Bureau. Sivaraman:Incyte: Employment. Colucci:Incyte: Employment, Equity Ownership. Yao:Incyte: Employment. Mascarenhas:Celgene: Membership on an entity's Board of Directors or advisory committees; Promedior: Research Funding; CTI Biopharma: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Research Funding; Merck: Research Funding; Incyte: Membership on an entity's Board of Directors or advisory committees, Research Funding; Roche: Research Funding; Janssen: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal